Tools and Resources
Maximus contracts to provide online PASRR Level I and Level II IDD screening and online Level of Care utilization review for long-term care populations.
Stay connected to important program updates and helpful program resources. If you aren't currently on the Indiana PASRR contact list, please reach out to the Help Desk with your name and facility name: 833.597.2777 | pasrr@fssa.in.gov
Your feedback helps us improve! Tell us about your assessment experience.
Are you a Qualified Mental Health Professional or Registered Nurse with behavioral health experience interested in becoming an Independent Contractor with the IN PASRR program? We are also seeking Licensed Psychologists to conduct IQ Testing.Contact our recruiting team to learn more: Recruiting@maximus.com
If you are interested in direct hire employment opportunities within the IN PASRR program or other Maximus clinical programs, please visit https://maximus.com/clinical
NOTE: The 1135 waiver PASRR approval is no longer in effect as of May 12, 2023. All PASRR assessments must be done before any admission to a nursing facility (preadmission).
7:30 am - 4:00 pm EST, M-F
Announcements
- Learning Opportunity: Review Quarterly PASRR Provider Webinar Recording to Learn More About Launch of Level of Care Assessment Representative (LCAR) Services | Explore Transition Next Steps
The Indiana Family and Social Services Administration (FSSA) and selected partner, Maximus continue to move toward the upcoming launch of the Indiana Level of Care Assessment Representative (LCAR) Services. As announced in an earlier communication, these changes will bring new innovations and a comprehensive, integrated approach to several of the State’s assessment services.
The introduction of LCAR Services will be a two-phased approach. Phase I process changes, which FSSA anticipates for a July 1 implementation, will focus on adding a Managed Care Entity (MCE) role so that Level of Care (LOC) assessments can be completed by MCEs for anyone in the PathWays Waiver. No significant changes will occur for most stakeholders currently involved in PASRR referral submissions. Your PASRR help desk support team contacts and website also remain unchanged.
In Phase II, Maximus will begin conducting Level of Care Assessments on individuals seeking nursing facility care, individuals in the PathWays Waiver, the TBI Waiver, and the Health and Wellness Waiver. Additionally, Maximus will provide Options Counseling and Medicaid Application Assistance. More will be shared about the timeline and next steps for Phase II later this year.
Note: LCAR will not be doing LOC assessments or Options Counseling for the CHOICE program.
NEXT STEPS: LCAR Services – Phase I TransitionMaximus has begun LCAR Services training sessions for MCEs, ensuring they’re prepped for their new role in the LOC assessment process. We will continue to keep all PASRR program stakeholders aware of the transition’s progress in the months ahead of the State’s anticipated July 1 implementation for Phase I.
LEARN: Review Recent Quarterly PASRR Provider Webinar PresentationThank you to everyone who was able to join the Quarterly PASRR Provider Webinar on Thursday, March 28. If you were unable to attend or would like a refresher on the topics covered during this informative one-hour session, please click on the links below to watch a video and review the presentation to learn more about LCAR Services.
- Quarterly PASRR Provider Webinar | Video – 59:30 mins
- Quarterly PASRR Provider Webinar | Presentation Slides
SUPPORT: Contact the Help Desk
Please contact the Indiana PASRR Help Desk team to assist you with any PASRR related questions:
- Email: pasrr@fssa.in.gov
- Phone: 833.597.2777
Resources are also available to providers on the PASRR Tools and Resources site:
- Quarterly PASRR Provider Webinar | Video – 59:30 mins
- Program Update: Exciting Changes Ahead with Planned Launch of Level of Care Assessment Representative (LCAR) Services | Review Next Steps | Register for Quarterly Webinar
On behalf of the State of Indiana Family and Social Services Administration (FSSA) and your support team at Maximus, we’re pleased to announce an exciting evolution ahead for the PASRR program, as well as other assessment services and resources that help ensure that individuals across the State receive the supports they need.
In the months ahead, numerous State agencies and service entities will work together toward the launch of the Indiana Level of Care Assessment Representative (LCAR) Services. These changes will bring new innovations and a comprehensive, integrated approach to assessment services.
What’s changing?A two-phase approach will be used for the LCAR Services implementation.
- LCAR – Phase I
Phase 1 will add a Managed Care Entity (MCE) role so that Level of Care (LOC) assessments can be completed by MCE providers for anyone in the Pathways Waiver. The State currently anticipates implementation of this new process on July 1, 2024.
- LCAR – Phase II
Maximus will begin conducting Level of Care Assessments on individuals seeking nursing facility care, individuals in the Pathways Waiver, TBI Waiver, and the Health and Wellness Waiver. Additionally, Maximus will provide Options Counseling and Medicaid Application Assistance. More will be shared about the timeline and next steps for Phase II later this year.
What’s not changing?There are no significant changes planned with the LCAR Phase I implementation for most stakeholders currently involved in PASRR referral submissions. Your PASRR help desk support team contacts and go-to resources site, https://MaximusClinicalServices.com/SVCS/Indiana will also remain unchanged.
What’s next for the LCAR transition?As Maximus and the State team move forward with outreach and MCE training, we also know that the continued support of community partners like you will be invaluable to help ensure the LCAR transition process is a success for all program stakeholders and the populations we serve together.
Keeping you informed throughout the transition is one of our most critical goals. Learn more below about the Quarterly PASRR Provider Webinar planned for March 28 and the LCAR-related topics to be covered during this one-hour session. Stay tuned for additional updates as we move closer to the State’s anticipated implementation of Phase I process changes on July 1, 2024.
Register to learn more about the LCAR implementationJoin us for the informative Quarterly PASRR Provider Webinar. We will discuss some upcoming process changes for Level of Care screens and some other important PASRR reminders. There will also be time for Q&A with our project team during this informative one-hour session. A recording will be made available after the session for individuals unable to attend.
Who do I contact with PASRR process or system-related questions?As always, please contact the Indiana PASRR Help Desk team to assist you with any PASRR related questions:
- Email: pasrr@fssa.in.gov
- Phone: 833.597.2777
Resources are also available to providers on the PASRR Tools and Resources site:
- LCAR – Phase I
- Learning Opportunity: Register for Upcoming PASRR Q&A Session on December 13
Join the Maximus - Indiana PASRR team for answers to all of your toughest PASRR questions. We won't be presenting new information or training, so bring your questions with you. Our team will answer as many questions as time allows.
After registering, you will receive a confirmation email containing information about joining the webinar.
SUPPORT: Contact the Indiana PASRR Help DeskDo you have PASRR process or system-related questions? Contact the Indiana PASRR Help Desk team:
- Email: pasrr@fssa.in.gov
- Phone: 833.597.2777
- Quarterly Provider Newsletter: Assessment Best Practice Tips & Reminders | Review Resources on Indiana Provider Site
BEST PRACTICES: Assessment Tips & Reminders
1. A new PASRR or Level of Care is not required if there is a current one, if there has not been a status change, and if the individual is returning to a nursing facility.
2. Keep in mind that a Level of Care is required for Medicaid, when Medicaid is pending, and whenever a Level II is required.
TOOLKIT: Review Important Guides and Training Materials Available on the IN PASRR Provider Tools & Resources SiteKeep in mind that the Indiana PASRR Provider Tools & Resources site is full of helpful guides, manuals, and training materials that you can view or download 24/7. Be sure to review a few of these helpful resource links also listed below:
- Indiana PASRR FAQ for Providers
- Indiana PASRR - Level of Care Reimbursement Process
- IN PASRR Provider Training: PASRR Process and Level I
- Being Ready for a Level II: Questions and Information Needed from Providers - Slides
- Being Ready for a Level II: Questions and Information Needed from Providers - Recording
- Indiana: PASRR and Processes - Slides
- Indiana: PASRR and Processes - Recording (Register to view, when prompted)
SUPPORT: Contact the Indiana PASRR Help DeskDo you have PASRR process or system-related questions? Contact the Indiana PASRR Help Desk team:
- Email: pasrr@fssa.in.gov
- Phone: 833.597.2777
- Indiana PASRR FAQ for Providers
- Important Process Reminder: Level of Care Added to PathTracker Admission Modal
Keep in mind that nursing facility users now must select the appropriate Level Of Care (LOC Short or Long) assessment on the PathTracker Admission modal when admitting Medicaid recipients to their respective nursing facilities.
The Level Of Care (LOC Short or Long) assessment selected should correspond to the timeframe matching the individual’s initial length of stay for the particular admission in question (see screenshots below):
PathTracker Admission Modal: 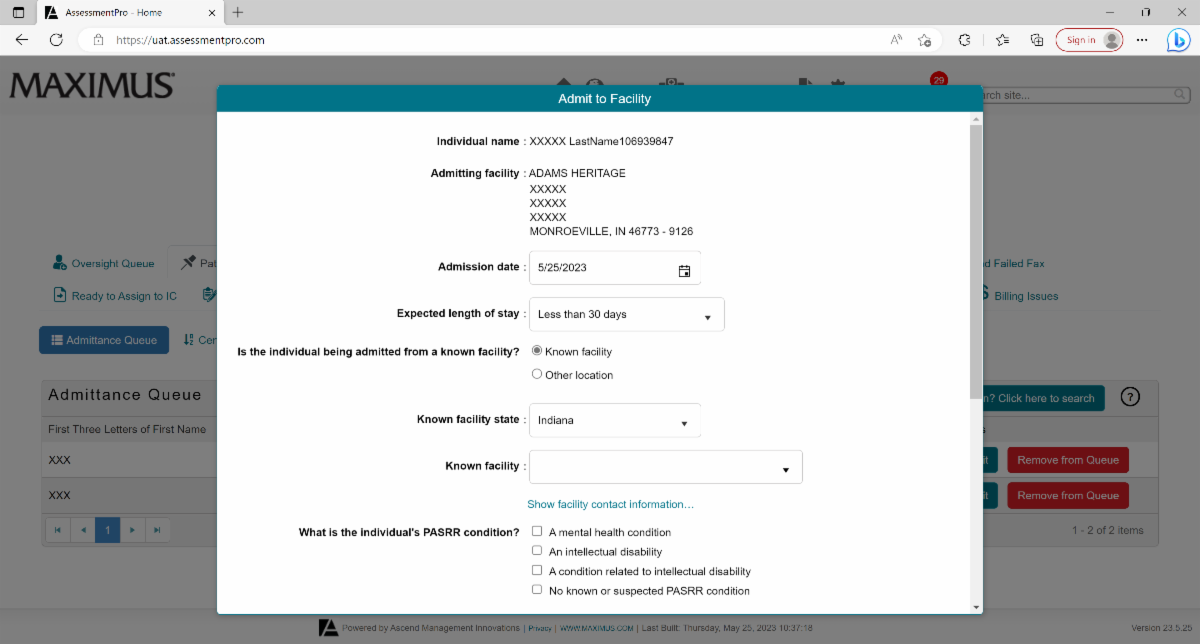
Select the assessment for this admission:

This will ultimately assist in the streamlining of the automated payment processing system for nursing facility Medicaid reimbursement. To avoid payment issues or disruptions, it is important to select the Level Of Care (LOC Short or Long) assessment that was submitted for the individual’s particular nursing facility stay.
We will be making further enhancements in the future to improve the user experience in this regard, and will send out additional communications at that time.Thank you for your attentiveness and cooperation with this new procedure. If you have any questions about this important update, please contact the IN PASRR Help Desk at 1.833.597.2777 or email pasrr@fssa.in.gov.
SUPPORT: Contact the Indiana PASRR Help Desk
If you have other questions about this upcoming change and how it will affect PASRR activities, please contact the Indiana PASRR Help Desk:Email: pasrr@fssa.in.gov
Phone: 833.597.2777 - Quarterly Provider Newsletter: Register for July 27 Q&A Session | Important Process Update | Best Practice Tips & Reminders
REGISTER: IN PASRR Provider Q&A Session | 2:00 p.m. ET on Thursday, July 27
What PASRR related topics would you like to learn more about? What questions can we answer for you? Join the IN PASRR team for a Q&A session on Thursday, July 27 at 2:00 p.m. ET. There's no prepared presentation, no recordings, no lecture - just a chance for us to answer your questions.
Click the link below to register in advance for this informative session:
IN PASRR Q&A Discussion | 2 p.m. ET on Thu, July 27
PROCESS UPDATE: DOA Waiver is No Longer a Substitute for the LOCPlease be aware that going forward, an uploaded waiver will no longer stand as substitute for Level of Care (LOC). A short form LOC is needed in addition to the attachment of the Division of Aging waiver. This excludes BDDS community waivers for MFP/CIH.
BEST PRACTICES: Assessment Tips & Reminders- To help with timely completion of Level II assessments, please fax in all documentation requested by Assessors. This helps the Level II Clinicians complete your summary of findings and reudces turnround times. Some items an Assessor may ask for include:
PT/OT notes
Medication Administration Records (MAR)
Psychiatric notes or evaluations
Keep in mind that documentation must be faxed directly to Maximus from the facility, and cannot be sent via email or taken offsite by an Assessor. Likewise, any mental health diagnosis used in a Level II must come from a document signed by a Medical Doctor or Nurse practitioner, and must have been completed within the past year (i.e. psychiatric evaluation or progress note, H&P or medical progress note)
- Remember that submitters are always expected to respond to contact attempts to schedule Level II assessments and participate in the interview. If the submitter of the Level I/Level of Care is not the person Maximus should contact to schedule and participate in the Level II, then the appropriate contact's information should be noted in the Level I communication box or notes section. If we cannot reach the facility or hospital to schedule the assessment, the assessment may be cancelled, and the submitter will have to resubmit.
- Be sure to check your email for the digital Scheduling Attestation and Release of Information forms submitted by Assessors for signature. This form is used to confirm that the Assessor completed the interview at the facility and to ensure aRelease of Information is signed, where applicable.
SUPPORT: Contact the Indiana PASRR Help DeskEmail: pasrr@fssa.in.gov
Phone: 833.597.2777 - To help with timely completion of Level II assessments, please fax in all documentation requested by Assessors. This helps the Level II Clinicians complete your summary of findings and reudces turnround times. Some items an Assessor may ask for include:
Resources
- 2023 Announcements - Archive
- 2022 Announcements - Archive
- 2021 Announcements - Archive
- 2020 Announcements - Archive
- Indiana PASRR - Provider Manual
- Guide: Using Secure Email
- Indiana PASRR Glossary of Terms
- Indiana PASRR FAQ for Providers - Updated on 4.21.21
- Indiana PASRR - Level of Care Reimbursement Process
- Editing System User Email Address - AP Administrator
- Editing System User Email Address - System User
Guides & Forms
Education & Training
- IN PASRR Provider Training: Introducing LCAR and PASRR Reminders - Slides
- IN PASRR Provider Training: Introducing LCAR and PASRR Reminders - Recording (59:30)
- IN PASRR: Revisiting AssessmentPro and Level I - Slides
- IN PASRR: Revisiting AssessmentPro and Level I - Recording
- IN PASRR Provider Training: PASRR Process and Level I
- Being Ready for a Level II: Questions and Information Needed from Providers - Slides
- Being Ready for a Level II: Questions and Information Needed from Providers - Recording
- Indiana: PASRR and Processes - Slides (1.11.22)
- Indiana: PASRR and Processes - Recording (1.11.22)
- Indiana PASRR Webinar (Slides) 10.1.2020